Table of Contents
- Introduction: When Protection Turns Into Exhaustion
- What Is PTSD and When Does Trauma Become a Disorder?
- What Changes in the ‘PTSD Brain’ (Smoke Detector vs Watchtower)?
- What Is Neurofeedback, and How Can It Help PTSD?
- How Do Alpha and Theta Waves Relate to Trauma Recovery?
- What Research and Meta-Analyses Say About Neurofeedback for PTSD?
- What Happens During a PTSD-Focused Neurofeedback Session?
- Which Neurofeedback Protocols Are Commonly Used for PTSD?
- How Does Brain Mapping (qEEG) Personalize Treatment?
- Is Neurofeedback Safe for PTSD, and How Does It Compare to Other Treatments?
- What Results Should I Expect and How Are They Measured?
- Can I do Neurofeedback at Home, or Do I Need to Come In?
- What Does a Realistic 10–12-Week Plan Look Like?
- What If I Don’t Feel Different Right Away? (Common Troubleshooting)
- How Long Do Benefits Last, and What Does the Evidence Say About Longevity?
- How Is Neurofeedback Different From “Just Relaxation” or Apps?
- Conclusion: Relearning Safety From the Inside Out
Introduction: When Protection Turns Into Exhaustion
After trauma, the brain does what it was built to do: protect you. It becomes hyper-vigilant, scanning the horizon for threat. But staying “on guard” 24/7 is exhausting. Stress chemistry ramps up, attention narrows, sleep frays, and everyday triggers can feel like alarms. Over time, this survival mode can reshape neural activity itself, affecting memory, impulse control, and emotional balance. The hopeful news: those changes are trainable.
Neurofeedback uses real-time EEG feedback to help the brain relearn calm regulation. Paired with psychotherapy, it can reduce arousal, restore sleep, and widen your window of tolerance. Below, we walk through what changes in the PTSD brain, how neurofeedback works, what the research says, and how treatment looks in practice, locally in Ontario and worldwide.
What Is PTSD and When Does Trauma Become a Disorder?
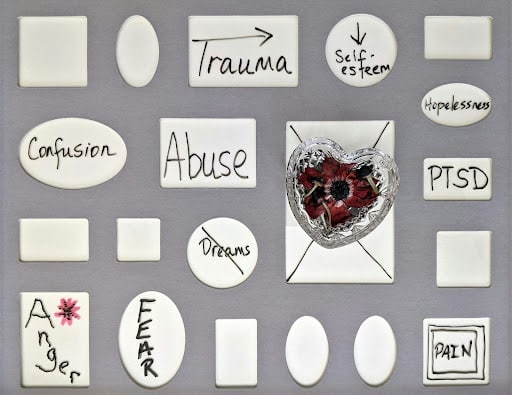
Everyone has stress reactions after terrifying or overwhelming events, nightmares, intrusive images, jumpiness, trouble concentrating. For many, these ease over weeks as the nervous system recalibrates. Post-traumatic stress disorder (PTSD) is when symptoms persist and impair daily life: re-experiencing (flashbacks/nightmares), avoidance, negative shifts in mood and beliefs, and hyperarousal (irritability, poor sleep, exaggerated startle).
What Happens in the Brain After Trauma?
Trauma sensitizes threat-detection circuits and weakens the brain’s braking systems. The result is a nervous system that learns fear too well and can’t easily down-shift. EEG and neuroimaging studies show reduced alpha power (less cortical “idling”/inhibition), increased fast-arousal signals, and changes in connectivity across control networks, patterns strongly linked to hyperarousal and attention capture by threat cues.
What Changes in the ‘PTSD Brain’ (Smoke Detector vs Watchtower)?
Which Brainwave and Network Patterns Are Affected?
A helpful metaphor (popularized by trauma clinicians) is the amygdala as the brain’s “smoke detector” and the medial prefrontal cortex (mPFC) as the “watchtower.” In PTSD, the detector fires easily; the watchtower struggles to quiet the alarm. That imbalance drives the body’s stress response (racing heart, fast/shallow breathing, muscle tension) and crowds out thoughtful evaluation.
On EEG, this often appears as:
- Lower posterior alpha and/or elevated fast activity, a neural signature of chronic alerting.
- Disrupted alpha–theta balance, reducing access to relaxed yet aware states that support integration and memory reconsolidation.
- Altered network connectivity (e.g., Default Mode Network and Salience Network), which can normalize as symptoms improve.
These are correlations, not diagnoses, but they’re actionable. If we can help the brain spend more time in balanced rhythms and less time in alarm states, symptoms often ease.
What Is Neurofeedback, and How Can It Help PTSD?
Neurofeedback is a form of EEG biofeedback. Small sensors on the scalp record (not stimulate) brain activity. Software converts that activity into immediate auditory/visual feedback (a movie brightens or sound becomes smoother when your brain trends toward targeted patterns). Your nervous system learns through operant conditioning, to reproduce those calm, efficient patterns more easily.
How Does EEG Feedback Work in Real Time?
- Measurement: EEG sensors detect moment-to-moment brain rhythms.
- Feedback: The app/game responds instantly to shifts.
- Learning: Rewards reinforce balanced activity; the brain repeats it.
- Generalization: With practice, regulation carries over into daily life.
What Brain Patterns Does Neurofeedback Target for Trauma Recovery?
For PTSD, protocols typically aim to reduce hyperarousal, restore alpha rhythms, and improve network coordination underlying attention and emotion regulation. Randomized trials and meta-analyses now report moderate, clinically meaningful symptom reductions for PTSD with EEG-based training, with benefits extending to anxiety and depression as secondary outcomes.
How Do Alpha and Theta Waves Relate to Trauma Recovery?
Two rhythmic players matter a lot in trauma work:
- Alpha (≈8–12 Hz): relaxed alertness; supports cortical inhibition (filtering noise) and calm focus.
- Theta (≈4–8 Hz): inward, imagery-rich states; appears in deep relaxation and some meditative phases.
PTSD often features reduced alpha (too little “calm gating”) and unstable alpha–theta dynamics. Protocols that increase alpha and/or rebalance alpha–theta can lower anxiety and support processing of traumatic material without overwhelm. Meta-analytic and RCT data suggest alpha-based neurofeedback can reduce PTSD severity and normalize connectivity within control networks.
Why Is Alpha/Theta Training Particularly Relevant for PTSD?
Alpha-Theta training gently guides the brain into a relaxed, imagery-friendly theta state and then toward alpha dominance, allowing traumatic memories to surface in a safe, deeply calm context and reconsolidate with less threat. In a landmark program with Vietnam veterans, Peniston & Kulkosky reported striking reductions in PTSD symptoms and medication use compared to treatment as usual; benefits persisted with follow-ups and booster sessions. While early, small-sample methods have limitations by modern standards, these studies catalyzed decades of development and continue to inform practice.
Today’s evidence base is broader: RCTs (e.g., van der Kolk et al., 2016) and recent meta-analyses indicate moderate beneficial effects overall and highlight alpha-modulation as a viable protocol class for PTSD.
What Research and Meta-Analyses Say About Neurofeedback for PTSD?
- A 2016 randomized controlled trial in chronic PTSD found significant symptom reductions following neurofeedback, with changes aligned to EEG markers of arousal (reduced alpha, elevated theta/alpha ratio) and improved affect regulation.
- A 2023 systematic review/meta-analysis reported moderate improvements in PTSD symptoms across RCTs and linked clinical gains to network-level changes (Default Mode and Salience Networks) following alpha-modulating protocols.
- A 2023 open-access review summarizing RCTs and mechanisms similarly found neurofeedback reduced PTSD symptom burden and comorbid anxiety/depression, with evidence pointing to normalization of connectivity and arousal rhythms.
- A 2024 meta-analysis of RCTs confirmed significant symptom reductions versus control conditions (sham/active/wait-list), while encouraging further standardization of protocols and outcome measures.
Takeaway: Research suggests that neurofeedback may help some individuals with PTSD improve emotional regulation, reduce stress-related arousal, and support recovery when used alongside other treatments. Studies are also exploring how it may influence brain networks related to memory, attention, and mood. Larger trials with standardized protocols will continue to clarify its potential benefits.
What Happens During a PTSD-Focused Neurofeedback Session?
Set-up (5 minutes): The clinician places small EEG sensors; the software confirms signal quality.
Baseline (2–3 minutes): Brief rest to set individualized thresholds.
Training (20–30 minutes): You watch a movie or view simple graphics that brighten/continue when your brain trends toward the target state (e.g., more mid-alpha; smoother low-beta) and dim/pause when it drifts into hyperarousal or rumination.
Cool-down (2–5 minutes): Breathing, grounding, or a short check-in to consolidate the calmer state.
Frequency: Typically 2–3 sessions/week. Many programs plan 20–40 sessions, with tapering and optional boosters. Early gains often appear in sleep and startle/reactivity, followed by improved attention and emotional balance.
Which Neurofeedback Protocols Are Commonly Used for PTSD?
There isn’t a one-size-fits-all method; mapping and symptoms guide choices. Examples:
Feeling Anxious or On Edge?
Explore how anxiety may be showing up for you and discover ways to regain calm.
- Alpha-increase / alpha-asymmetry balancing: Restore calm gating and left-right regulation.
- Alpha-Theta (A-T): Deep relaxation and safe recall/reconsolidation of traumatic memories.
- Infra-Low Frequency (ILF) neurofeedback: A very slow-signal approach designed to stabilize arousal regulation and network timing; early literature and case series suggest value in trauma populations.
- SMR/low-beta stabilization: Improves sleep onset, sensory filtering, and body calm.
- Connectivity-oriented training: Targets coordination between sites to support executive control over limbic arousal (an emerging research area).
Clinicians often blend methods over time, beginning with stabilization, then adding A-T or connectivity work once sleep and daytime calm improve.
How Does Brain Mapping (qEEG) Personalize Treatment?
Before (or early in) training, many clinics record a quantitative EEG (qEEG) at rest (eyes open/closed). Software compares your frequency patterns and synchrony with age-matched norms to spotlight dysregulated sites/frequencies (e.g., reduced posterior alpha, excess fast-beta frontally, asymmetric alpha, or unstable theta).
Why map?
- It targets the plan (which bands/sites to emphasize).
- It tracks change (objective pre/post measures).
- It clarifies when to shift protocols (e.g., from stabilization to A-T).
qEEG isn’t a diagnosis, but it’s a powerful compass for individualized care.
Is Neurofeedback Safe for PTSD, and How Does It Compare to Other Treatments?
Standard EEG neurofeedback records only; it does not apply current to the brain. Side effects are uncommon and usually mild/temporary (brief fatigue, “spacey” feeling early on). Good practice includes clinician supervision, careful thresholding, and gradual progression.
How it fits with therapy:
- Psychotherapy (CBT/EMDR/trauma-informed): “Top-down” tools for meaning-making and exposure.
- Neurofeedback: “Bottom-up” self-regulation of arousal so therapy is tolerable and effective. RCT authors note that improved affect regulation can reduce drop-out from exposure-based care
- Medication: Can be combined; some clients later adjust meds with their prescriber as regulation improves.
What Results Should I Expect and How Are They Measured?
Early signs include fewer nighttime awakenings, less startle, calmer baseline, and quicker recovery after triggers. Over sessions, many report:
- Decreased intrusive images/nightmares
- Less “on edge” muscle tension
- Improved concentration and task follow-through
- Greater ability to be present (less scanning/dissociation)
- More flexible emotional responses
Clinics track both physiological metrics (time-in-target, artifact rate, stability of trained bands) and functional markers you care about (sleep quality, number of “spikes”/day, time to settle after triggers). Ideally you see progress across three independent indicators (physiology + self-report + behavior) before calling a change real.
Can I do Neurofeedback at Home, or Do I Need to Come In?
Home-capable EEG systems exist. A hybrid model often works best: clinic-based assessment and protocol design, followed by supervised home sessions with regular reviews to tweak thresholds and ensure signal quality. This expands access in Whitby/Durham Region and beyond without sacrificing precision.
What Does a Realistic 10–12-Week Plan Look Like?
Weeks 1–2 (Stabilize & Learn): 2–3 sessions/week. Focus on sleep, startle, and daytime steadiness.
Weeks 3–6 (Build Capacity): Continue stabilization; consider adding gentle A-T or ILF once sleep is reliable. Start brief “transfer routines” (2-minute breathing + orienting) before daily stressors.
Weeks 7–10 (Generalize): Increase complexity (connectivity targets; context-specific sessions). Add psychotherapy exposures or skills practice while the nervous system stays inside the window of tolerance.
Weeks 11–12 (Consolidate & Taper): Space sessions; confirm gains hold between visits. Plan maintenance (e.g., monthly boosters during high-stress seasons).
What If I Don’t Feel Different Right Away? (Common Troubleshooting)
- Check adherence: Consistency (2–3×/week) matters more than intensity.
- Verify signal quality: Hair/gel/contact/movement artifacts can mask learning; clinicians adjust placement and impedance.
- Right difficulty: Thresholds too easy/hard can stall progress—fine-tune for ~60–75% reward.
- Layer supports: Sleep timing, light exposure, hydration, and gentle movement all boost neuroplasticity.
- Sequence wisely: For complex trauma, stabilize first; add A-T or exposure only when your window of tolerance is wider.
How Long Do Benefits Last, and What Does the Evidence Say About Longevity?
Follow-ups in classic and modern studies report sustained symptom reductions months after training, particularly when clients complete a full course and integrate skills (breathing, grounding, paced exposure). Some opt for booster sessions during anniversaries or transitions. The long-term literature continues to grow, but the trend toward durable change, not just transient relief, is one of neurofeedback’s potential benefits.
How Is Neurofeedback Different From “Just Relaxation” or Apps?
Many tools lower stress in the moment. Neurofeedback is different: it trains neural regulation itself with real-time brain-based feedback. Studies tie clinical gains to measurable EEG/network changes (e.g., alpha restoration; DMN/SN connectivity shifts), evidence of systems-level learning, not just a placebo or distraction effect.
How Do I Choose an Ethical, Qualified Provider in Ontario?
Look for clinicians who:
- Use a structured assessment (often qEEG) to personalize your plan.
- Explain what they’re training and why, with realistic timelines.
- Track objective metrics and functional goals you define together.
- Collaborate with your therapist/physician (CBT/EMDR/med management).
- Avoid “cure-all” claims; practice within scope and emphasize safety.
In Ontario (Whitby, Durham Region, GTA), The Insight Clinic offers qEEG-informed neurofeedback integrated with psychotherapy. That blend (data + relationship + skills) is where long-term change tends to stick.
Conclusion: Relearning Safety From the Inside Out
PTSD is not “all in your head”, it’s in your nervous system. Trauma reshapes rhythms and networks that govern how you feel, focus, and sleep. The same neuroplasticity that wired survival mode can rewire ease, presence, and connection.
Neurofeedback gives the brain a mirror and a map:
- a mirror (feedback) that shows when it’s calm and connected, and
- a map (qEEG/metrics) to track progress and adjust course.
Combined with compassionate therapy, it may turn recovery into learned regulation rather than white-knuckling. The goal isn’t to erase the past; it’s to teach your brain that the danger is over, so you can live where your life is, here and now.
If you’ve been feeling on alert long after the danger has passed, know that change is possible, and you don’t have to navigate it on your own. Schedule a FREE 15 min neurofeedback consultation to learn how personalized brain training may help support your healing process. Take a step toward the version of yourself you’re working to become.